“A Blood Test Saved My Life” says young cancer patient

Lowering HbA1C Levels To Less Than 7% Increases Life Expectancy In Diabetics By 3.8 Years
The advantages of better glycemic management on diabetes patients’ quality-adjusted life years have long been understood. It is also well-accepted that better glycemic control management aids in preventing problems associated with diabetes.
A recent study has now stressed on a direct relationship between tighter glycemic control and longer life with results showing an approximate 3.8 years increase in the life expectancy of diabetics with an achieving lower HbA1C levels of lower than 7 per cent.
The management of diabetes involves a multidisciplinary approach, including health care professionals, appropriate goal settings, dietary and exercise modifications, medications, and monitoring of blood glucose and complications. (1)
Having type-2 diabetes (T2D) is linked to a 6-year reduction in life expectancy at age 50 compared to those without the disease. In T2D patients, better control of blood pressure, glucose, cholesterol, and body weight may lower the risk of diabetes-related morbidity and mortality, lengthening life expectancy.
Relationship Between Glycated Hemoglobin and Life Expectancy (1)
A recent JAMA study has shown a direct relationship between glycemic control and longer life expectancy.
A US-based study led by Kianmehr et al. at the University of Florida, Gainesville, conducted a survey to quantify potential gains in life expectancy among T2D patients associated with lowering HbA1C, low-density lipoprotein cholesterol, systolic blood pressure (SBP), and body mass index toward optimal levels. For this purpose, they used the BRAVO (Building, Relating, Assessing, and Validating Outcomes) diabetes model.
This finding is expected to significantly impact the advocacy for tightening glycemic control among T2D patients since it directly relates the health benefit of blood sugar control with longer life expectancy. Clinicians can use these results to encourage patients to meet suggested treatment objectives and to assist in prioritizing initiatives and programs to enhance diabetes management.
The study enrolled 421 US nationals with self-reported diagnosed diabetes by a clinician, where the data were analyzed over the course of 10 months by grouping the study population into quartiles based on levels of glycated hemoglobin (HbA1C), systolic blood pressure (SBP), low-density lipoprotein cholesterol (LDL-C), and body mass index (BMI).
The study led to the following findings:
- Among 421 individuals, 46% were women, and the mean age was 65.6 years.
- In type 2 diabetes patients, lower BMIs of 24.3 (first), 28.6 (second), and 33.0 (third) were respectively associated with 3.9, 2.9, and 2.0 additional life-years compared with a BMI of 41.4 (mean of the fourth quartile).
- Lower systolic blood pressure levels of 114.1 mm Hg (first), 128.2 mm Hg (second), and 139.1 mm Hg (third) were tied to 1.9, 1.5, and 1.1 years gained in life expectancy in type 2 diabetes patients, respectively, compared with an SBP of 160.4 mm Hg (fourth).
- A lower LDL-C level of 59 mg/dL (first), 84.0 mg/dL (second), and 107.0 mg/dL (third) were tied to 0.9, 0.7, and 0.5 years gain in life expectancy versus LDL-C of 146.2 mg/dL (fourth).
- HbA1C reduction from 9.9% (fourth) to 7.7% (third) was linked with 3.4 years of gain in life expectancy. However, a further decrease to 6.8% (second) was tied to only a mean growth of 0.5 years in life expectancy, and from 6.8% to 5.9% (first) was not linked to life expectancy benefit.
- A life expectancy gain of 3.8 years was seen with a reduced HbA1C from the fourth quartile to the first.
These results were in line with the ACCORD trial, which found that lowering the treatment goal for HbA1C to less than 6% in high-risk patients reduced the number of 5-year nonfatal myocardial infarctions. However, patients who did not meet the treatment goal had a higher 5-year mortality rate.
These studies emphasize a heatmap of predicted remaining life years by age and risk factor level that may be used as a clinical reference to promote collaborative decision-making with patients.
They also stress the necessity of biomarker management at a younger age and the potential requirement of a trade-off between treatment and life quality for T2D patients when the value of biomarker control is minimal.
Assessment of Glycemic Control: Glycemic control is assessed by the A1C measurement, continuous glucose monitoring (CGM), and self-monitoring of blood glucose (SMBG). The latest Standards of Medical Care in Diabetes released by the American Diabetes Association recommends assessing glycemic status (A1C or another glycemic measurement) at least two times a year in patients who are meeting treatment goals (and who have stable glycemic control).
The guideline further recommends preprandial blood sugar levels of 90 to 130 mg/dl and a hemoglobin A1C (HbA1CP) level of less than 7% as an ideal checkpoint
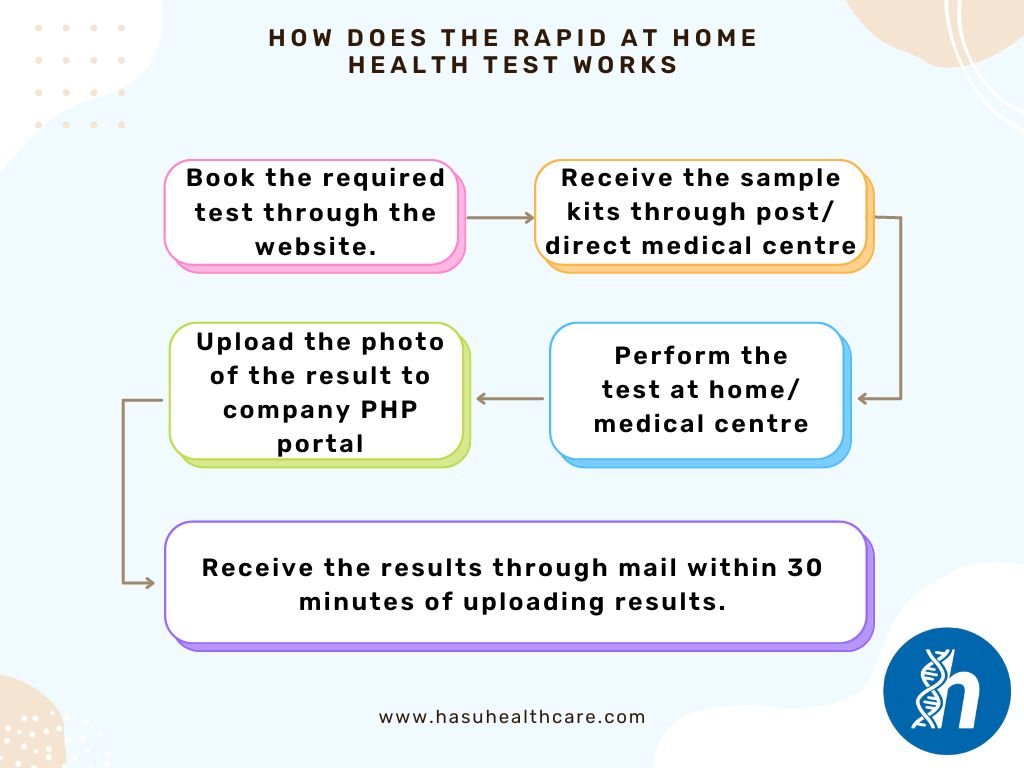
- If your test is Rapid and you have booked and tested at Medical Centre you will your test results in 30minutes after your test , A clinical staff will provide you verbal outcome of your test.
- If you test is run through the postal then a clinical team will call you or sent you an email after received your sample by post and laboratory has performed the test.
- For fit to fly RT-PCR or Antigen test the result will be sent to you by your email as a PDF copy, please check your email inbox, junk box or spam folder the email comes from Hasu Health care.
- Result times vary depending on the test that has been booked.
• The Rapid test has over greater than 96 % sensitivity and 99% specificity for the Biomarkers, the Rapid test tells you whether you have enough level of the Biomarkers or not as Qualitative test. And in most of cases that information is sufficient to alert you for the condition at early stage to start the necessary measures to prevent your conditions to develop further.
MIND you the RAPID test is ALERT you for the under lying conditions you may be unaware of.
We will provide the Diagnosis of the test you have performed and provides you suggestions, the most common suggestion is to contact your GP or your Doctor and ask them that you have run the Rapid test and needs the further investigation.
You can ask our GP service which is Chargeable for £40 per consultation which can be 15 minutes call.
- With postal services they can normally take up to 48 Hours (2 working days) to arrive at our medical centre. (Note the tracking number given on the return label).
- Following table provides overview of the expected results of the postal samples

- Please note that postal services are not operational on Sunday and Bank Holidays, we may receive the kits from the next working day onwards.
- You can organise your own courier/postal service. Postal address is given on the blue card.
- Yes you can with Our Barclay Card Payment system you can Pay using Credit/Debit Card.
- The order number is the Reference to your Purchase which you would receive in your email After the Payment of the test as a Order confirmation email
- The test barcode is Reference to your Sample which is found on the Sample tube and corresponding cards that are sent to you
- For the Preparation of sampling
- Wash or sanitise your hands.
- Follow the Instruction provided on back of the Blue Test Card
- Place the Sample tube back into the box with the Registration Card (purple card) and Keep with you the Blue Test card for your reference
- Stick the provided prepaid Royal Mail returns label onto the return bag.
- Post in a Royal Mail Priority Post Box only.
- Please see our Refund Policy